What if you could DOUBLE the positive impact at HALF THE COST of most current “wellness” models? What if you could truly get your population engaged (over 80%), and have over half of your population improve their health, without any incentives? Wouldn’t that be worth considering?
While most large employers in the U.S. say they offer a wellness program, less than 7% use all the program components required for successful interventions (Goetzel & Ozminkowski, 2008). So, chances are, you are throwing money at an under-performing employee health promotion program.
The greatest weakness in most health promotion strategies is that the interventions are designed for the wrong people. Most interventions are built to accommodate people at advanced stages of behavioral readiness. The problem is, the vast majority of people are at early stages of readiness, and unfortunately, simply raising their awareness or incenting them to minimally engage will not magically advance them to the stage of sustainable action.
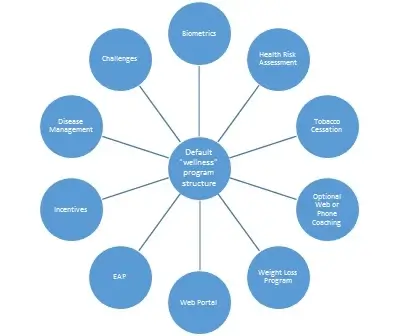
The “default” wellness strategy of most large organizations is a hub and spoke model like this (click here).
I understand the logic – “people have different needs and interests, so let’s put together an array of options to cover all our bases…”
Unfortunately, most of these bases are never reached. They require an employee to proactively choose to engage (e.g. opt in, log on, make a call, fill out a form, or attend something outside of their normal work and routine).
As you can imagine, being proactive is not a characteristic of someone at an early stage of readiness (i.e. most of your workforce). Even if you get someone to participate, the expectations or actions within the individual programs are short term, or also oriented to people who are ready to make a change. And finally, even for those who do participate in some activities within this model, travel within this framework is a constant “out and in”. That is, it is rare for the different elements of the program to cohesively reinforce each other or actively encourage flow around the circle from one activity to the next. The result is that overall engagement is low, and repeat consistent engagement across different activities (which is most likely to reinforce and facilitate change) is even lower.
These downfalls lead us to incentives. When traditional “wellness” wasn’t working, rather than address the flaws in the model, the great epiphany was to introduce incentives. Again, I see the logic – “we have all these great programs available, if only people would use them…so let’s use incentives and challenges to make it fun and rewarding, and everything will be fixed, right?…”
Well, it turns out that works initially…but it’s superficial and unsustainable. People can be easily enticed to make short term shifts or episodic changes, but these rarely translate into meaningful sustained change because you haven’t appropriately taken an individual through a complete, inherent change process. So as soon as the incentive is removed or is no longer appealing, or as soon as a non-routine stressful interruption happens in someone’s life, they inevitably revert back to their old poor behaviors. Why? Because the episodic behavior was never inherently driven or meaningful – and as soon as it’s no longer convenient, it’s terminated.
That brings us to the current state of our industry. The majority of workplace health promotion programs are vastly under-performing, yet companies continue to increase incentives or chop and change vendors in an attempt to make marginal improvements – all while slowly losing faith that any of it is worth the effort (or cost) – and all while slowly extinguishing any limited motivation their workforce may have had. According to SHRM, the average wellness incentive is now just shy of $600 per head per year. That’s a really poor investment of wellness budgets which could more effectively be spent on better interventions.
In any other aspect of business, if you determine there is an ineffective process, do you continue to invest more money to marginally improving that flawed process, or do you look to innovate and correct the process? Einstein is often credited with a definition of insanity to the effect of “doing the same thing over and over while expecting a different outcome.” So I ask, are American businesses completely insane?
If people are not effectively utilizing your program without incentives, it DOES NOT mean you should tinker with different incentive models, IT DOES mean that you have the wrong program.
Low effective engagement without incentives is a clear sign that your employees do not see inherent value in your program. Therefore, you need to change your program, and what the science tells us is, you need approaches which are easier for people at earlier stages of behavioral readiness. Remove the proactive “opt-in” barriers, reduce the clutter of excess, narrowly-focused programs, and create a basic process of consistently and repeatedly delivering short – sharp bits of relevant, actionable health information to your whole population.
If budget permits and methods of appropriate coaching that allow the information to be tailored and delivered relevant to an individual’s personal needs and stage of readiness, then the impact is even greater. You can still have other relevant targeted interventions available for those that need them, but people’s progress towards those more advanced interventions should be nurtured and supported – not coerced.
At HBD, we’ve rethought the health promotion model. We’ve de-cluttered it – because that makes it simple and more relevant for people at earlier stages of behavioral readiness. We try to filter out the noise, and create a clear, structured process for more consistently “drip-feeding” relevant and progressive education using fun, non-threatening themes which help re-frame complex health concepts. We work to integrate the education and engagement into the normal work flow so that people don’t have to opt-in, and we adjust the content so that it’s relevant depending on individual interests, needs, and stage of readiness. While additional resources for high risk individuals may still be necessary (e.g. PCP, EAP), moving people to an appropriate stage of readiness before referring them to these services will make the interventions more successful. This more successful health promotion model is more linear (click here) and provides greater consistency and continuity, making engagement and action far more sustainable.
So if your health promotion strategy looks like the hub and spoke model: stop. If the value of your annual wellness incentives are more than $100 per head: stop. If challenges or incentives are the only things that are keeping your program alive: stop. There is little long term value in continuing to battle for marginal improvements within that flawed system. Instead, reinvent the system, and redistribute that wellness budget into something that will actually make a difference, and that your employees will actually get satisfaction and value from.
You have very little to lose from at least giving us the time for a conversation. If the idea of DOUBLING your program effectiveness while potentially reducing the investment at all peaks your curiosity, then try giving us a call or visit the “contact us” page and send us an email.